
I Had a Cleft Lift and it Failed
Am I Doomed? The short answer is, “no”. But, what should you do now? When a cleft lift fails – meaning that either the incision came apart and isn’t healing, or a new cyst, sinus, or wound has…
Read more
Am I Doomed? The short answer is, “no”. But, what should you do now? When a cleft lift fails – meaning that either the incision came apart and isn’t healing, or a new cyst, sinus, or wound has…
Read more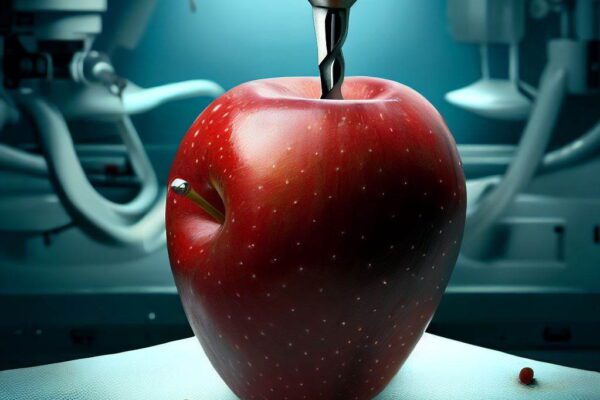
The Gips Procedure is one of the many pilonidal operations that fall into the “minimally invasive pilonidal surgery” category. This procedure is a modification of the Bascom pit picking procedure, and…
Read more
Is this something I need to worry about? Often patients ask if they need to worry that untreated pilonidal cysts or sinuses will turn into cancer. The short answer is “probably not”. But there are some…
Read more
A new age of internet search is upon us! In the past, we could search Google, Bing, Yahoo, etc, and these search engines would take us to thousands (if not millions) of web pages discussing the topic we…
Read more
This week, Dr. Norbert Zapotoczny joined me from Wroclaw, Poland to refine his cleft lift skills. Dr. Zapotoczny is already an experienced cleft lift surgeon, but wanted to collaborate on technique. We…
Read moreWe routinely take care of patients with pilonidal cysts, non-healing pilonidal wounds, and pilonidal abscesses with great success in the pediatric, teen, and adult age groups.